Source: Washington State ATrainATrain-1

| Home | Air leakage | Materials |
| SiteMap | Orders/Manufacturers | Contact Us |
Some scientific research has tried to get approximate "minimum infective dose" (MID) quantities of various pathogens, including viruses Yezli-1. For example, for many viruses and other pathogens, if you get a smaller dose, then you might not get infected, or you might get infected but not very sick, or you might get sick but not die. As regards the COVID-19 coronavirus, there is a lot we don't know, but we may assume it's generally the same as for other viruses, that you don't need 100% protection.
Reducing the dose of the COVID-19 coronavirus may:
A face mask which works only partially works, by not stopping all virus but still stopping a significant percent of COVID-19 coronaviruses, may still offer significant propylactic protection and be well worth wearing.
For example, of people worldwide confirmed to be infected with the COVID-19 coronavirus, look at the very low death rate of people in Asian countries where face mask usage is very high, which is very different from western countries where face mask usage has been very low. I suspect it's because people in Asia are getting lower infective doses.
A small infection may be able to trigger the immune system enough to keep the infection under control, but a heavy initial dose such as hanging around an infected person for a long time, or getting a big initial dose from a cough, could quickly overwhelm the body before the immune system has a chance to detect the new pathogen and ramp up to fight it.
Therefore, partial protection from the COVID-19 coronavirus might make a significant difference in whether or not you get infected at all, how contagious you might get, if you get sick then the severity of your illness, and whether you live or die.
For some other pathogens, there is a lot of scientific data from research. There are lots of pathogens in drinking water, foods, and other sources which do not cause symptomatic infection because they are less than a minimum infective dose, and there are resultant standards in the industry for allowable levels of some pathogens. The water you drink and the food you eat is not 100% free of pathogens. There just aren't enough to hurt you, usually.
For the COVID-19 coronavirus, there is no such data as far as I know regarding infective dose and severity of infection vs. initial dose. There are no simple answers to these questions for the COVID-19 coronavirus at this time. However, it's still interesting to read research on other viruses.
It appears that approximately half of all infected people do not get sick, i.e., are asymptomatic. For example, research in the small town of Vo, Italy, which had an outbreak, whereby they locked down the town of 3300 and tested everybody, 100% of the population, sick or not, found that 89 people were infected, but only about half of them showed symptoms of sickness. Similar results have been found elsewhere.
It is now believed that many people who have no symptoms may be spreading the virus further.
Scientific studies have found viruses being shed out into the air not just from coughs, but also from just breathing.
Let's go thru this step by step.
People tend to have the largest amount of virus in their system before their immune system starts to control it. The virus replicates and spreads quickly before the immune system ramps up, so that the concentration of virus in the body can get very high, but then is brought down by the immune system.
This means people can be contagious before they are sick, and more contagious before a strong reading on an antibody test. A test to detect the virus directly, instead of detecting antibodies, is more important in measuring how contagious a person is. (In other words, a PCR test is more important than an antibody test, in measuring how contagious a person is, during the early stage of infection.)
A newly infected person who is not sick at all could be much more contagious than an infected person who just has a fever and is not yet coughing.
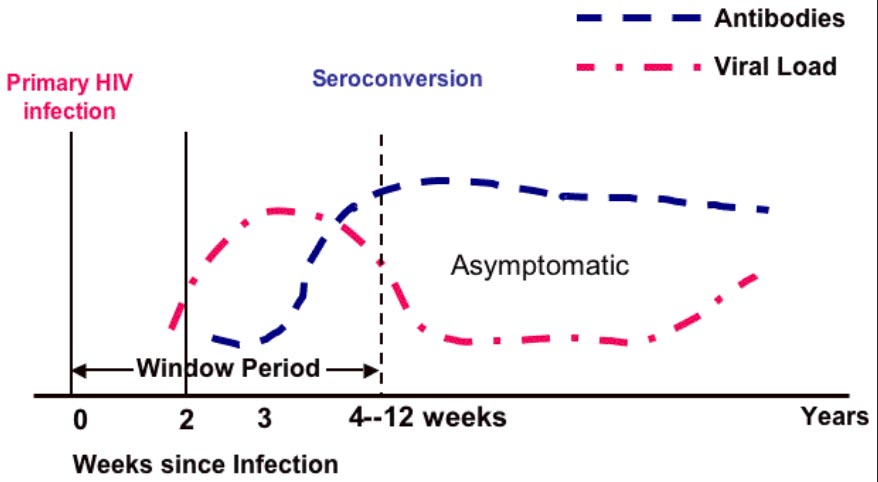
Some people may remember about HIV, which causes AIDS. When a person was first infected, they were more contagious to others, before antibody tests gave a strong reading. In the graph below, the red line is the "viral load" -- the number or concentration of viruses in the body. The blue line is antibodies -- the number or concentration of antibodies. As you can see, early during an infection, in the first several weeks, the level of virus is highest, so the person is most contagious. The virus level comes down as the antibodies level rises.
Source: Washington State ATrainATrain-1
Note also that an antibody test can come up negative during the early phase when the viral load is high but antibodies have not yet been produced.
I chose HIV as an example because it's another infection of high interest to people. COVID-19 is similar, except you can squeeze the curve down to days instead of weeks or years.
Here's for another virus called BTV which might have a profile more similar to a coronavirus like COVID-19 as regards the actual number of days:
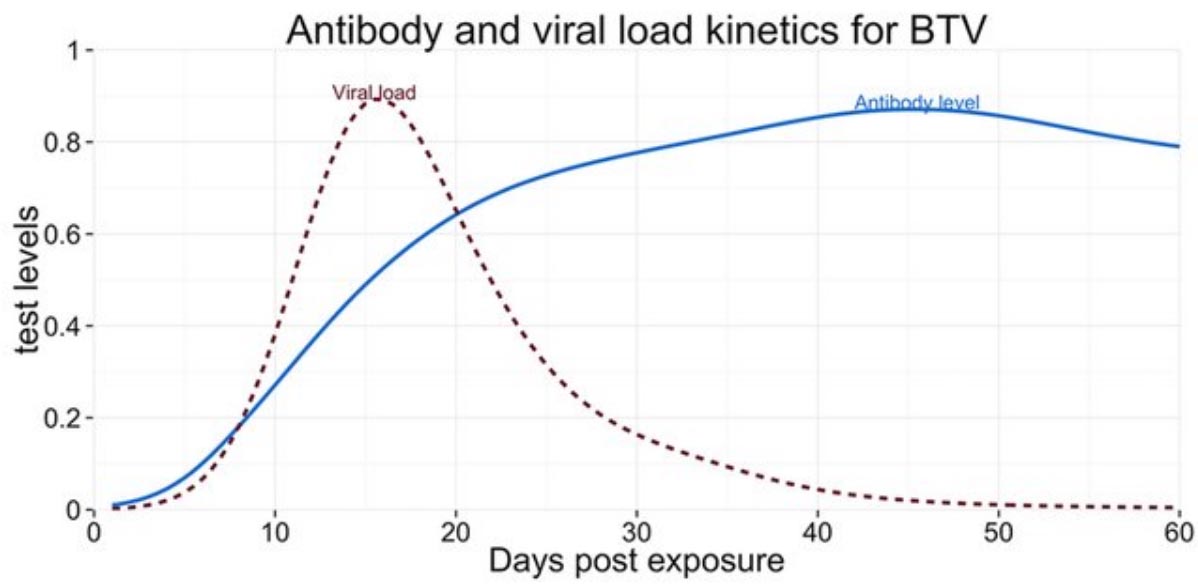
Source: Rydevik et al.Rydevik-1
Just because a person is not sick does not mean they cannot give you the virus. Many experts think that people with no symptoms at all -- asyptomatic (don't get sick) or pre-symptomatic (do get sick but later) -- might be a major source of infections of others, for the COVID-19 coronavirus.
This is why everybody must wear a mask and practice social distancing even when there are no symptoms of anybody being sick ... yet.
There isn't much in depth data on COVID-19 from just breathing, but there is some interesting laboratory work on the shedding of other respiratory viruses, which found that "Of the 25 subjects who had virus-positive nasal mucus, the same virus type was detected in 12 breathing samples, 8 talking samples, and in 2 coughing samples. ... These data provide further evidence that breathing may be a source of respirable particles carrying infectious virus."Stelzer-Braid-1
Particles of size 4 micrometers and less (4000 nanometers) can remain suspended in air and spread over a larger distance. The smaller the particle, the longer it will stay suspended, and the further it can travel.
Also, particles of size 4 micrometers and less can penetrate deeper into the lungs when breathed, and it is thought that the infections dose can be much lower this way. "... two reviews of previous studies concluded that the infectious dose by the aerosol route is likely considerably lower than the infectious dose by intranasal inoculation [2,8], and that aerosol inoculation results in more severe symptoms [8], presumably because aerosol particles are able to deposit deeper in the respiratory tract." Lindsley-et-al-1 Weber-Stilianakis-1 Tellier-1
The extra infectiousness of smaller particles means we must emphasize the need for face masks to filter the smaller particles.
Another scientific study found that 60% of patients with influenza A had detectable levels of viral RNA in just their exhaled breath. Not coughing, not talking, just exhaling. Of the exhaled particles, over 87% were less than 1 micrometer (1000 nanometers) in diameter. Fabian-1
This was consistent with research by another group of scientists of influenza infected people, which split particles into larger and smaller than 5 micrometers, with the smaller particles holding 8.8 times more virus than the larger particles. However, what I found most interesting in this study is that the number of viruses in the finer particles was much higher on day 1 of onset of influenza symptoms, and fell on days 2, 3, and 4. This was by about a factor of roughly 10 times for the median reading, but by a factor of about 295 times for the maximum reading, which is consistent with the early peak of shedding before antibodies bring the viral rate down, but also raises the issue of super spreaders by the big difference between median and maximum readings. The researchers also noted and discussed this. Milton-1
Other studies show a very wide variation in viral shedding by different people, which further raises the issue of super spreaders.
The above research by Milton et al. was just for breathing. For people coughing, the particle sizes and virus concentrations are different. For example, in one study, 35% of all influenza RNA measured was contained in large particles of 4 microns or larger in diameter, 23% was in 1 to 4 micron diameter particles, and the largest amount, 42%, in cough particles less than 1 micron in diameter.Lindsley-et-al-1
So, whether an infected person is breathing or coughing, it's the smallest particles we need to be able to filter the most.
The above research indicates that the smaller particles are most infectious of the lungs and thus may have a much smaller "minimum infective dose", and they're also the most abundant as regards carrying the virus, but a third factor also comes into play -- smaller particles linger suspended in the air for a much longer period of time, and can travel much further distances.
Another study generated COVID-19 aerosol particles using a machine instead of human coughs, and then did tests on them to see how long the COVID-19 would remain viable.
For the aerosols, they tested for just 3 hours, and stated "SARS-CoV-2 remained viable in aerosols throughout the duration of our experiment (3 hours) ..." van-Doremalen-1
In my own analysis, it may be expected that aerosol particles will disperse due to air flow, so that going beyond 3 hours doesn't make much practical sense unless you are in a small sealed room or somewhere like that. Outdoors, air disperses quickly, and in shopping malls, superstores, and other places there should be considerable circulation from air conditioning. However, inside a small air conditioned room such as in a home or small shop, the virus can linger in relatively high concentration for a long time.
Think of what a place is like with a smoker. Then imagine the smoke smell being a virus.
Much of the virus will eventually collide with and stick to things such as walls, clothes, items on grocery store shelves, and so on, to further reduce the concentration in the air. For example, think of the smell of cigarette smoke on your clothes.
Not all virus particles have the same life time. Most humans might live to be between 70 and 90 years old, which is a relatively a narrow range, but viruses are not the same, as the same virus can be tested as viable for between 1 hour and 72 hours, depending upon whether they are in the air or on a particular surface, and other conditions. Therefore, it is important to understand the meaning of "half-life", which is when half of all particles are no longer viable. For example, if a particle has a half-life of 1 hour, then:
After 1 hour, only half the particles will be viable, i.e., 50%.
After 2 hours, only half that 50% will still be viable, i.e., 25% of the original sample.
After 3 hours, only half that 25% will still be viable, i.e., 12.5% of the original sample.
(As an analogy to illustrate half life, let's imagine that somebody says the half life of a marriage is 10 years. These are made up numbers about marriage, not based on any actual survey, but just to make a point. A 10 year half life of marriage would mean that half of all people married would be divorced after 10 years, 25% of couples would make it to 20 years, and 12.5% would make it to 40 years. If you wanted to manufacture and sell greeting cards to celebrate a particular anniversary, such as "Happy 20th Anniversary!", within a particular local jurisdiction, then you might want to make an analysis of your market to see what would be profitable enough -- financially viable. Just because only 12.5% make it to 40 years, that might still be a "minimum infective dose" if the local market population is large enough.)
For COVID-19, the half lives were approximately:
1.1 hours to 1.2 hours in aerosol
On copper surfaces, the half life was similar to aerosol
5.6 hours on stainless steel
6.8 hours on plastic
Widely variable on cardboard (such as shipping boxes), in between copper and stainless steel van-Doremalen-1
With half-lives this long, viable concentrations of virus can linger for days on some surfaces. We can't say a given number, because it depends on the initial dose of virus, such as how much somebody is shedding and how they are transmitting it, but one of the numbers bouncing around on the internet is up to 3 days for some situations and items. It also depends on the temperature, humidity, and maybe some other factors.
For example, some people are reusing surgical masks without disinfecting and cleaning them, out of concern that cleaning and disinfecting may damage the mask, so they may rotate them by setting them aside for a long time, hoping that the quantity of viable viruses will eventually be below a minimum infective dose. Alternatively, they might instead want to put them in an oven at 60C for longer than a recommended time of 30 minutes. We can't say that all viruses are destroyed after 30 minutes, but we can say that a lot more are destroyed after 30 minutes than after 1 minute.
These results emphasize the need to be careful what you touch, and clean your hands after potential exposure, long after the air may dissipate.
However, an indication of just how much a virus can spread in the air comes from a news report of a church choir gathering of 60 people on March 10 in a jurisdiction which did not yet have any reported cases. The meeting announcement by the conductor on March 6 mentioned about the "stress and strain of concerns about the virus ..." but said they would go ahead and meet on March 10, and they apparently felt safe enough to meet. They practiced social distancing, avoided handshakes and hugs for the most part, had hand sanitizer at the door, and everybody came with their own sheet music. They were together for about 2.5 hours. Some people interviewed afterwards said nobody was coughing nor appeared sick. Out of the 60 people, 45 turned up COVID-19 positive nearly 3 weeks later -- 75% !! Of those, 2 were dead and 3 more hospitalized. This was reported on March 29. LA-Times-1
All this makes me question just how effective current social distancing guidelines are, in that many of them say just 6 feet or 2 meters, especially in indoor areas. Many people think they can just walk around with no face mask as long as they stay 2 meters away from others, including indoors! The government gives people a space number, and many people think it's that simple. I have watched COVID-19 press conferences in mid-April 2020 of people not wearing masks just practicing approximately 6 foot distancing indoors, together for a long time. What kind of example is that for the general public?
This page is on minimal infective dose, and analysis surrounding that. On this page, I'll stick to the science of minimal infective dose and transmission. However, there are also politics, governments, leaders, and cultures, as discussed on other pages.
If you want to see my political critiques on some governments, the World Health Organizations (WHO), and some cultures, regarding handling of the COVID-19 situation, then that's on other pages, such as Comments / Opinion. However, over time, my confidence in many governments has gone further and further down.
However, more importantly, I've also been very concerned about the potential of biotechnology and synthetic biology to create a far worse pathogen in the future, whereby COVID-19 is just a very mild practice run. After all, the eventual death rate may be well be use a few percent. It may wreck the economy and push health care systems to the extreme, but things could be far worse for the human species in the not so distant future. This has been my focus since the 1980s, actually. Also, since my confidence in governments has continued to decline steeply for about 40 years now, I'm focused almost entirely on the private sector.
I suggest you also see the brief page on this website on Future Pandemic Risks.
You are currently here:
![]() Face-Mask-Sealer.com > Minimum infective dose
Face-Mask-Sealer.com > Minimum infective dose
You may contact us via our contact page.

|
Lucky Lion Pride Co., Ltd. 69/1049 Moo 3 Bungyeetho Thanyaburi Pathum Thani 12110 THAILAND |

|
|
Copyright © 2019-2026 by Mark Evan Prado, All Rights Reserved.
Parts of this website are derived from my pollution mask work in 2019. |
| Home | Air leakage | Materials |
| SiteMap | Orders/Manufacturers | Contact Us |
